Bimonthly assessment for February 2021
This is my submission of the assessment of February 2021
Link to the current assignment is below:
https://medicinedepartment.blogspot.com/2021/02/medicine-paper-for-february-2021.html?m=1
1Q. 50 year old man, he presented with the complaints of
Frequently walking into objects along with frequent falls since 1.5 years
Drooping of eyelids since 1.5 years
Involuntary movements of hands since 1.5 years
Talking to self since 1.5 years
Link to the case presentation:
https://archanareddy07.blogspot.com/2021/02/50m-with-parkinsonism.html?m=1
And link to the case discussion:
a. What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
PROBLEM PRESENTATION:
Regular alcoholic and tobacco chewer
An episode of GTCS seizures 10 years back
Diagnosed as diabetic 2 years back when he had fall from bike and got his leg fractured and was operated
Difficult to keep his eyes open and the difficulty is progressing since 1.5 years
Changes in behaviour as described by his wife like self talking and being reserved unlikely to his normal behaviour as of being aggressive since 1.5 years
Started walking in to things and only looks straight ahead and involuntary movements of bilateral hands which is on and off only while doing work since 1.5 years
Diagnosed with hypokalemia and is on supplementation since June 2020
Thin stream of urine and bed wetting since one year
ANATOMICAL LOCALISATION:
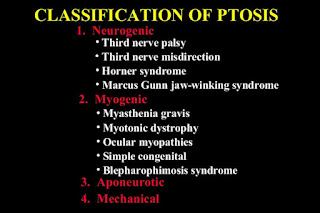
Bilateral ptosis: weakness of Levator palpebrae superioris
Self talk : frontal lobe
Vertical gaze palsy :
Mostly it is supranuclear palsy
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Problem representation:
H/O CVA 2 years back on medication weakness of limbs improved but loss of speech persisted
Shortness of breath grade 4 according to NYHA with Orthopnea and PND since 2 months
Bilateral Pedal edema up to ankle along with abdominal tightness and discomfort since 2 months
Oliguria along with burning micturition since 2 months
C/o generalised weakness along with pain in bilateral lower limbs since 2 months
Anatomical localisation:
Based on history :
Sob orthopnea and PND indicates left heart failure due to atherosclerosis
Risk factors for atherosclerosis include
Elderly age ( 60 years)
Alcohol intake
Hypertension
Based on examination:
shift of apex to 6th ics,presence of thrill palpable at apex(?s1), nature of the apex not mentioned
presence of loud p2 ,dilated veins ,pedal edema,s3 in both apical and left parasternal areas.
(?biventricular failure)
Time line of events :
Episode of CVA with persistent loss of speech since 2 years
Shortness of breath, PND, orthopnea bilateral pedal edema , oliguria since 2 months
b. What is the efficacy of each of the drugs listed in his current treatment plan?
1. Salt and fluid restriction:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4282615/
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
)?Sub acute combined degeneration of spinal cord secondary to vit B12 deficiency.
?Diabetic neuropathy
?Hypervolemic hyponatremia secondary to heart failure
?Pseudohyponatremia secondary to uncontrolled sugars
c) What is the efficacy of each of the drugs listed in his current treatment plan especially for his hyponatremia? What is the efficacy of Vaptans over placebo? Can one give both 3% sodium as well as vaptan to the same patient?
tolvaptan vs placebo
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3573862/
Hyponatremic patients in the SALT-1 and SALT-2 studies with a diagnosis of SIADH were identified based on clinical diagnosis by individual study investigators. Subjects were randomized to receive oral placebo (n=52) or tolvaptan 15 mg daily, with further titration to 30 and 60 mg daily, if necessary, based on the response of serum [Na+] (n=58).
In patients with SIADH, improvement in serum [Na+] was significantly greater (P<0.0001) with tolvaptan than placebo over the first 4 days of therapy as well as the entire 30-day study, with minimal side effects of increased thirst, dry mouth, and urination. Only 5.9% of tolvaptan-treated patients had overly rapid correction of hyponatremia as defined by current guidelines. After discontinuation of tolvaptan, serum [Na+] declined to values similar to placebo. A significant positive treatment effect favoring tolvaptan on the physical component, and a near-significant trend on the mental component, was found using the SF-12 Health Survey. Tolvaptan was associated with a significantly reduced incidence of fluid restriction.
https://www.sciencedirect.com/science/article/pii/S0085253815557803
This review focuses on why hyponatremia should be treated and the role of these antagonists in the treatment. Upon analysis of the available literature, we conclude that there is presently no role for vaptans in acute symptomatic hyponatremia. Although numerous therapeutic approaches are available for chronic symptomatic hyponatremia, vasopressin antagonists provide a simpler treatment option. Vaptans are efficacious in raising serum sodium in long-standing ‘asymptomatic’
3%NACL and tolvaptan
https://link.springer.com/article/10.1007/s00228-020-02848-6
From a total of 77 patients included in the analysis, 24 (31.2%) showed sodium overcorrection (> 10 mmol/L/24 h); 2 (2.6%) in heart failure cohort, 17 (22.1%) in SIADH cohort, and 5 (6.5%) in unknown cause cohort. More than half of patients (51.9%) were administered hypertonic saline prior to tolvaptan. Hypertension, cancer, diuretics, baseline serum sodium, and SIADH were associated with the risk of overcorrection in the univariable analysis.
from the above data,vaptans shouldnt be used in acute hyponatremia and prior administration of 3%NACL leads to over correction with the use of vaptan.
4) Please mention your individual learning experiences from this month?




Comments
Post a Comment